Now Reading: Components of Effective Diabetic Foot Care Plans
-
01
Components of Effective Diabetic Foot Care Plans
Components of Effective Diabetic Foot Care Plans

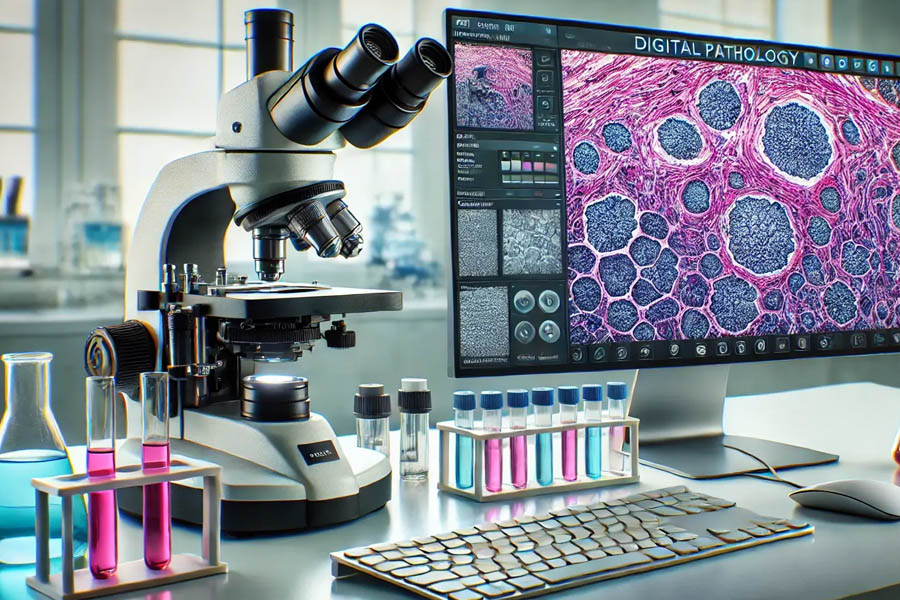
A podiatrist helps safeguard your foot health if you have diabetes. A diabetic foot care plan is a structured strategy designed to prevent complications, such as ulcers, that can limit mobility. Working with your foot doctor provides a collaborative approach to managing your condition. Key components of an effective diabetic foot care plan include:
Perform Daily Foot Inspections
When you visit your foot doctor, you undergo an examination to assess your nerve health and circulation. This evaluation helps identify early signs of complications that you might not feel due to nerve damage. Your foot doctor will give you specific instructions on what to look for and how to manage any changes in your feet.
Performing daily foot inspections helps you detect if there are any changes in your feet or toes. You can inspect your feet at night before going to bed, or in the morning before putting on socks and shoes. Some signs to look for include redness, swelling, blisters, cuts or sores, as well as changes in skin color or temperature. The earlier you detect these changes, the better your chances are of preventing cases of infection or other foot challenges.
Maintain Proper Foot Hygiene
Maintain proper foot hygiene by washing your feet daily with soap and water. Be sure to dry between your toes to prevent moisture accumulation in your shoes. After washing and drying, apply a moisturizing lotion to keep your skin soft and prevent cracking.
Your foot doctor inspects your skin for dryness, cracks, wounds, infections, or changes in texture during your visits. They also examine nail health and look for signs of fungal growth. Proper hygiene combined with professional inspection helps you protect your feet, detect problems early, and maintain healthy skin. Keeping your nails trimmed may also reduce the risk of ingrown nails or infections.
Manage Blood Glucose Levels
One component of a foot care plan is maintaining your blood glucose levels within your target range. Proper blood glucose control reduces the risk of nerve damage and poor circulation. Working with your foot doctor, you can develop a personalized management plan tailored to your specific needs, which may include regular monitoring of your blood sugar levels and guidance on diet, exercise, and medication.
Your foot doctor may also coordinate with your primary care provider or endocrinologist to verify that all aspects of your health are addressed. This collaboration helps in preventing foot problems before they develop. Maintaining healthy blood glucose levels supports better wound healing, reduces the risk of infection, and protects nerve and vascular health. By keeping your glucose levels stable, you are actively protecting your feet and preserving your mobility over time.
Wear Appropriate Footwear
When you are managing a diabetic foot condition, you need a comfortable pair of shoes that supports your daily activities. The appropriate footwear not only aids you in day-to-day activities but also safeguards your feet against injuries. Find shoes with additional cushioning and a wide toe box so that there is not too much friction or pressure on your feet. Tight shoes or high heels should be avoided, as they can cause blisters, calluses, and corns. Wear shoes that are breathable, such as leather or mesh shoes, to prevent your feet from getting wet. The heels of your shoes must also be well-formed to make sure that your foot is stabilized and aligned.
Visit a Foot Doctor for Foot and Ankle Conditions
Visiting a podiatrist helps prevent and manage foot problems. Regular check-ups, whether or not you have a diabetic condition, can help keep your feet healthy. Schedule an appointment for a routine exam or if you notice changes in your feet. A foot doctor provides expert guidance and personalized treatment plans depending on your goals.