Now Reading: Migraine Medications Explained: What Will Best Meet Your Needs
-
01
Migraine Medications Explained: What Will Best Meet Your Needs
Migraine Medications Explained: What Will Best Meet Your Needs
Understanding migraine timing and why it matters
Migraines have a rhythm of their own — some arrive like a siren, sudden and sharp, while others creep in hours after a rough night. That timing changes everything: a medication that works brilliantly when you catch a migraine early may feel sluggish if you wait until the pain peaks. Think of your migraine as a scene in a film; its pacing dictates which tool in your kit will create the right cut. Not every episode behaves the same, which is why one-size-fits-all thinking rarely helps.
Tracking how quickly your attacks escalate, how long they last, and whether they come with nausea or visual symptoms gives you a map. With that map you can match a medication’s speed, delivery method, and side-effect profile to the kind of episode you’re most likely to get. It’s not magic — it’s pattern recognition, and it gets sharper with a little attention.
How symptom patterns guide medication choice
When symptoms hit fast, you usually need something fast-acting. If they come on slowly, you can consider options that take a bit longer to unfold but last longer once they do. Some drugs have a rapid onset but shorter duration; others take longer but prevent rebound. Matching the pharmacology — how fast a drug is absorbed, how long it stays active — to your personal attack pattern increases the chance of a clean, decisive response.
Also, symptoms matter: if nausea is prominent, a swallowed tablet might not be the best route; if aura or visual disturbances precede pain, timing the dose during the aura can be helpful for some people. The trick is learning the choreography of your own attacks so you can step in with the right move at the right time.
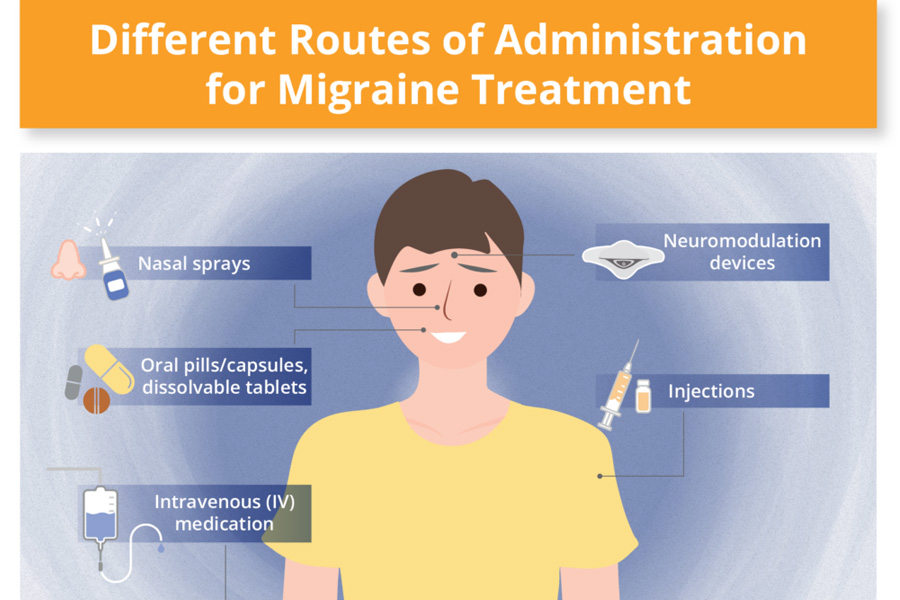
Formats and ease of use: tablets, liquids, dissolving strips
Format matters more than you might think. Tucking a dissolving strip in your pocket or having a quick-dissolve tablet in your wallet is different from fumbling with a bottle at the kitchen sink while light and sound are assaulting you. For people who feel queasy, non-oral routes like nasal sprays or dissolvable forms can bypass the stomach and act faster. Liquid formulations may absorb a little quicker than tablets; sublingual or orodispersible options remove the need for water — a small convenience that becomes monumental mid-attack.
Consider where you live your life. If you travel, work in meetings, or have kids, ease of use becomes a primary criterion. A medication that’s theoretically perfect but awkward to administer will often be used late or not at all, and that erodes effectiveness.
Comparing how different medications behave
There’s a whole cast of characters in acute migraine treatment: triptans (like eletriptan and rizatriptan), NSAIDs, antiemetics, and newer classes such as gepants and ditans. Triptans are a classic — fast and effective for many — but individuals vary in which triptan they tolerate or which one hits hardest. Eletriptan and rizatriptan may work differently for you depending on how the migraine unfolds and how quickly you take the medication.
NSAIDs can be reliable for milder attacks and are often used early; antiemetics help when nausea threatens absorption. The newer agents offer options for people who can’t take triptans because of vascular risk factors or who need something that won’t trigger medication-overuse headache as easily. The important point: different pharmacologic profiles exist, and the right choice is the one that lines up with your attack’s timing, symptoms, and safety needs.
Observe if certain triggers affect medication response
Triggers like sleep disruption, bright light, hormonal shifts, and stress don’t just start attacks — they can change how an attack behaves and how it responds to treatment. An attack triggered by sleep loss might feel heavy and slow, making longer-acting agents more useful; a stress-triggered lightning bolt might demand something with quick onset. Environmental factors can also alter how well oral medications absorb — for instance, if vomiting is present, an oral tablet may never reach full effect.
Keeping notes on what preceded each attack — what you ate, how you slept, what the weather did, how stressed you were — helps reveal patterns that affect both prevention and acute response. Over time, those notes often tell a clearer story than any single episode.
Adjust your method based on changing symptoms
Migraines can shift over months or years. A treatment that used to be a reliable rescue may become less helpful, either because the migraines themselves have evolved or because of side effects or overuse. When effectiveness declines, consider changing the dose form, switching within a drug class (for example, trying a different triptan), or exploring a newer class of medications. Tinkering slowly and with attention — rather than flipping strategies every attack — gives you data about what truly works.
If you find yourself taking acute medication very frequently, that’s a signal to reassess with your clinician: frequent use can lead to rebound headaches and diminishing returns. A measured approach — tracking frequency, timing, and response — keeps the options open and the outcomes better.
Keeping a headache journal: the practical rhythm
A headache journal is your forensic toolkit. Record onset time, symptom sequence, likely triggers, medication taken, format used, and how quickly relief arrived. Note side effects and whether relief was sustained or fleeting. Over weeks and months, patterns will emerge: which medications hit faster, which hold their effect, and which formats you actually reach for when the lights go out.
Simple consistency — a line or two after each attack — pays off. The journal turns anecdote into evidence, and evidence is the kind of thing that makes a tailored treatment plan possible.
FAQ
What’s the first thing I should consider when choosing a migraine medication?
Think about how quickly your migraines start and whether you have nausea or other symptoms that affect swallowing; timing and symptoms guide the choice between fast-acting versus longer-acting forms.
Are all triptans the same for everyone?
No — triptans share a mechanism but differ in speed, duration, and side-effect profiles, so one may work better for you than another.
When should I use a non-oral route like a nasal spray or dissolving strip?
Use non-oral routes if you have nausea, vomiting, or need a discreet, fast option that doesn’t require water.
Could triggers change how a medication works?
Yes — triggers can alter attack pace and severity, which in turn can affect how quickly and effectively a medication works.
How often is too often to take acute migraine medication?
Frequent use over weeks can lead to medication-overuse headache, so if you’re treating attacks very often, it’s time to reassess with a clinician.
Will switching formats (tablet to liquid) make a big difference?
Sometimes — format changes can improve absorption speed and practicality, and that can translate into noticeably faster relief for some people.
Should I compare eletriptan and rizatriptan directly?
Comparing two triptans can be useful, because personal response varies; trying one and then the other under similar circumstances helps reveal which fits your pattern.
How long should I track migraines before changing strategy?
Track consistently for several weeks to a few months to gather meaningful patterns, but seek help sooner if frequency or severity increases.